Sexual Problems
Sexology | Dr. Mahmood Yunus Usmani
Sexual Disorders
Expert care for sexual health
- Nocturnal Emission or Night Discharge
- Prematured Ejaculation
- Impotency
- Spermatorrhoea
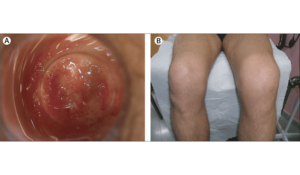
- Balanitis
- Herpes of Glans Pennis
- Orchitis
- Hydrocele
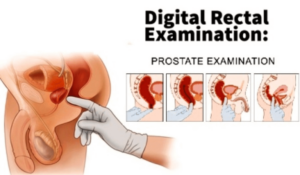
- Prostatitis
- Phimosis
- Scrotal Eczema
- Azoospermia
- Lymphogranuloma Vanereum
- Oligospermia
- Necrospermia
- Chancroid or Soft Chancre
- Non-Specific Urethritis

Nocturnal emission, commonly known as a wet dream or night discharge, is an involuntary release of semen during sleep. This natural occurrence is most prevalent among adolescent males but can also happen in adult men and, less commonly, in females. It typically transpires during REM (rapid eye movement) sleep and may or may not be accompanied by erotic dreams.
Causes:
Hormonal Changes: Increased testosterone levels during puberty can lead to spontaneous emissions.
Sexual Abstinence: Prolonged periods without sexual activity may result in nocturnal emissions.
Erotic Dreams: Sexual dreams can stimulate arousal leading to ejaculation during sleep.
Physical Stimulation: Friction from bedding or sleepwear may inadvertently cause arousal.
Symptoms:
Ejaculation During Sleep: Waking up to find evidence of semen release.
Damp Bedding or Clothing: Noticing wet spots on sheets or underwear upon waking.
Possible Erotic Dreams: Recalling sexual dreams that may have accompanied the emission.No Physical Pain: Typically, there is no discomfort associated with nocturnal emissions.
Prevention:
Regular Ejaculation: Engaging in sexual activity or masturbation can reduce the frequency of wet dreams.
Stress Management: Practicing relaxation techniques to minimize stress-induced emissions.
Proper Sleepwear: Wearing comfortable clothing to reduce unintended physical stimulation.
Healthy Sleep Patterns: Maintaining consistent sleep schedules to regulate REM cycles.
Nocturnal emissions are a normal part of human sexuality and development. If they cause distress or occur excessively, consulting a healthcare professional can provide reassurance and guidance.

Premature ejaculation (PE) is a common male sexual dysfunction characterized by ejaculation that occurs sooner than desired, either before or shortly after penetration, leading to distress for one or both partners. It affects men of all ages and can significantly impact sexual satisfaction and relationship quality.
Causes:
Psychological Factors: Performance anxiety, stress, depression, and relationship issues can contribute to PE.
Biological Factors: Hormonal imbalances, abnormal neurotransmitter levels, inflammation of the prostate or urethra, and genetic predispositions may play a role.
Erectile Dysfunction: Concerns about maintaining an erection can lead to a pattern of rushing to ejaculate.
Symptoms:
Rapid Ejaculation: Consistently ejaculating within a minute of penetration.
Lack of Control: Inability to delay ejaculation during intercourse.
Emotional Distress: Feelings of frustration, embarrassment, or avoidance of sexual intimacy.
Prevention:
Stress Management: Practicing relaxation techniques to reduce anxiety.
Open Communication: Discussing concerns with a partner to alleviate performance pressure.
Healthy Lifestyle: Maintaining regular exercise, balanced nutrition, and adequate sleep.
If PE persists and causes significant distress, consulting a healthcare professional is advisable for proper evaluation and guidance.

Impotence, also known as erectile dysfunction (ED), is the consistent inability to achieve or maintain an erection sufficient for satisfactory sexual performance. This condition can affect men of all ages and may lead to stress, reduced self-confidence, and strained relationships.
Causes:
Physical Health Issues: Conditions like diabetes, heart disease, high blood pressure, and obesity can impair blood flow or nerve function, leading to ED.
Hormonal Imbalances: Low testosterone levels or thyroid disorders can disrupt sexual function.
Neurological Disorders: Diseases such as multiple sclerosis, Parkinson’s disease, or spinal cord injuries can interfere with nerve signals necessary for an erection.
Medications: Certain drugs, including antidepressants, antihistamines, and blood pressure medications, may have side effects that contribute to ED.
Psychological Factors: Stress, anxiety, depression, and relationship issues can impact sexual performance.
Lifestyle Choices: Smoking, excessive alcohol consumption, drug use, and lack of physical activity can increase the risk of impotence.
Symptoms:
Difficulty achieving an erection.
Trouble maintaining an erection during sexual activity.
Reduced sexual desire.
Prevention:
Healthy Lifestyle: Regular exercise, balanced diet, and maintaining a healthy weight support vascular health.
Avoid Harmful Substances: Limiting alcohol, quitting smoking, and avoiding illicit drugs can reduce risk.
Manage Health Conditions: Controlling chronic diseases like diabetes and hypertension is crucial.
Mental Well-being: Addressing psychological issues and reducing stress through therapy or relaxation techniques can be beneficial.
Understanding the underlying causes of impotence is essential for effective management and prevention. If you experience persistent symptoms, consulting a healthcare professional is recommended for appropriate evaluation and guidance.
Spermatorrhoea, also known as Dhat syndrome, is characterized by the involuntary discharge of semen without sexual activity or orgasm. This condition can lead to physical discomfort and psychological distress.
Causes:
Excessive Sexual Activity or Masturbation: Overstimulation can lead to involuntary seminal discharge.
Psychological Factors: Anxiety, stress, and guilt associated with sexual thoughts may contribute.
Nutritional Deficiencies: Poor diet and lack of essential nutrients can weaken the body’s systems.
Weak Nervous System: Neurological issues may impair control over seminal emissions.
Prolonged Sexual Abstinence: Extended periods without ejaculation can result in involuntary release.
Physical Stimulation During Sleep: Contact with bedding or clothing may inadvertently cause arousal.
Symptoms:
Involuntary Semen Discharge: Occurs without sexual activity, often during sleep.
Fatigue and Weakness: Persistent tiredness and lack of energy.
Lower Back Pain: Discomfort in the lumbar region.
Irritability and Mood Swings: Emotional instability and frustration.
Loss of Appetite: Reduced desire to eat.
Burning Sensation in Genitals: Discomfort or irritation in the genital area.
Prevention:
Balanced Diet: Ensure adequate intake of essential nutrients.
Regular Exercise: Engage in physical activities to strengthen the body.
Stress Management: Practice relaxation techniques like meditation and yoga.
Avoid Excessive Sexual Activity: Maintain moderation in sexual practices.
Proper Sleep Hygiene: Establish a consistent sleep schedule and comfortable sleeping environment.
Understanding and addressing the underlying causes of spermatorrhoea can help in managing the condition effectively. If symptoms persist, consulting a healthcare professional is advisable.
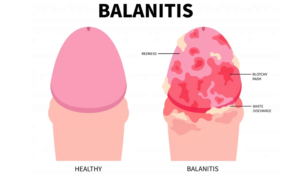
Balanitis is an inflammation of the glans penis, commonly affecting uncircumcised males. It can cause discomfort and may impact daily activities if left unaddressed.
Causes:
Poor Hygiene: Inadequate cleaning can lead to the accumulation of smegma, fostering bacterial or fungal growth.
Infections: Yeast (Candida), bacterial, or viral infections can trigger inflammation.
Irritants: Harsh soaps, detergents, or spermicidal products may cause allergic reactions.
Medical Conditions: Diabetes and other chronic illnesses can increase susceptibility.
Symptoms:
Redness and Swelling: The glans may appear inflamed and tender.
Itching or Burning Sensation: Discomfort during urination or sexual activity.
Discharge: A foul-smelling fluid may be present under the foreskin.
Pain: Especially during urination or erection.
Prevention:
Proper Hygiene: Gently retract the foreskin and clean the area with warm water daily.
Avoid Irritants: Use mild, unscented soaps and avoid harsh chemicals.
Manage Underlying Conditions: Keep chronic illnesses like diabetes under control.
Safe Sexual Practices: Use protection to reduce the risk of infections.
If symptoms persist or worsen, it’s advisable to consult a healthcare professional for appropriate evaluation and guidance.
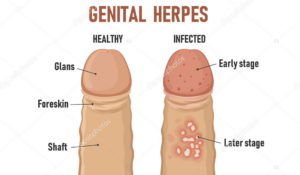
Herpes of the glans penis is a manifestation of genital herpes, a common sexually transmitted infection caused by the herpes simplex virus (HSV). It primarily affects the glans (head) of the penis, leading to discomfort and potential complications if left unaddressed.
Causes:
Herpes Simplex Virus Type 2 (HSV-2): Most genital herpes cases are due to HSV-2, transmitted through sexual contact.
Herpes Simplex Virus Type 1 (HSV-1): Typically causes oral herpes but can lead to genital infections via oral-genital contact.
Direct Skin-to-Skin Contact: Transmission can occur even without visible sores, through contact with infected skin or mucous membranes.
Symptoms:
Painful Blisters or Ulcers: Small, fluid-filled blisters on the glans that may rupture and form ulcers.
Itching or Tingling: Sensation often precedes the appearance of sores.
Redness and Swelling: Inflammation around the affected area.
Pain During Urination: Especially if sores are near the urethra.
Flu-like Symptoms: Fever, headache, and swollen lymph nodes during initial outbreaks.
Prevention:
Consistent Use of Protection: Using condoms can reduce, but not eliminate, the risk of transmission.
Avoid Sexual Contact During Outbreaks: Refrain from sexual activity when symptoms are present.
Regular STI Screenings: Early detection helps in managing and reducing spread.
Open Communication: Discuss STI status with partners to make informed decisions.
Understanding the causes, recognizing symptoms early, and taking preventive measures are crucial in managing herpes of the glans penis. If symptoms arise, consulting a healthcare professional is essential for proper evaluation and guidance.
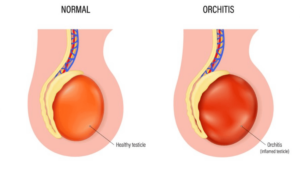
Orchitis is an inflammation of one or both testicles, often resulting from bacterial or viral infections. It can cause significant discomfort and, if untreated, may lead to complications affecting fertility.
Causes:
Viral Infections: Mumps is a common viral cause, particularly in post-pubertal males.
Bacterial Infections: Urinary tract infections or sexually transmitted infections like chlamydia and gonorrhea can lead to orchitis.
Epididymitis: Inflammation of the epididymis can spread to the testicles, resulting in epididymo-orchitis.
Other Factors: Infections such as brucellosis or tuberculosis may also cause orchitis.
Symptoms:
Testicular Pain and Swelling: Often sudden and severe, affecting one or both testicles.
Tenderness in the Scrotum: The scrotal area may be sensitive to touch.
Painful Urination or Ejaculation: Discomfort during these activities is common.
Fever and Malaise: Systemic symptoms like fever and a general feeling of unwellness may occur.
Enlarged Prostate: In some cases, the prostate may become enlarged.
Prevention:
Vaccination: Receiving the mumps vaccine can prevent viral orchitis.
Safe Sexual Practices: Using protection and regular STI screenings help prevent bacterial causes.
Prompt Treatment of Infections: Addressing urinary tract or epididymal infections early reduces risk.
Good Hygiene: Maintaining cleanliness can prevent the spread of infections.
Early recognition and management of orchitis are crucial to prevent complications. If symptoms arise, consulting a healthcare professional is essential for appropriate evaluation and care.
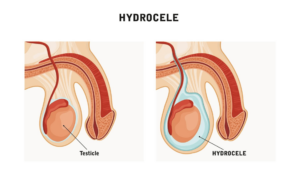
A hydrocele is a fluid-filled sac surrounding a testicle, leading to swelling in the scrotum. Common in newborns, it often resolves without intervention, but in adults, it may result from injury or inflammation.
Causes:
Congenital Factors: In infants, a hydrocele can occur when the processus vaginalis fails to close, allowing fluid to accumulate.
Injury or Trauma: Scrotal injuries can lead to fluid buildup around the testicle.
Infections: Inflammation from infections like epididymitis or orchitis may cause a hydrocele.
Post-Surgical Complications: Surgery in the groin or scrotal area can sometimes result in hydrocele formation.
Symptoms:
Scrotal Swelling: A painless, enlarged scrotum that may feel like a water-filled balloon.
Heaviness: A sensation of weight in the scrotum.
Discomfort: Large hydroceles may cause discomfort during movement or sexual activity.
Size Variation: Swelling might fluctuate throughout the day, often increasing with activity.
Prevention:
Protective Measures: Wearing appropriate protective gear during sports or activities can prevent scrotal injuries.
Prompt Treatment: Addressing infections or injuries promptly reduces the risk of hydrocele development.
Regular Check-ups: Routine medical examinations can help detect and manage conditions that may lead to hydroceles.
While hydroceles are generally harmless, persistent or large swellings should be evaluated by a healthcare professional to rule out underlying conditions and discuss potential treatment options.
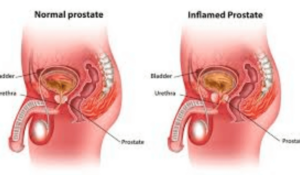
Prostatitis is an inflammation of the prostate gland that can cause urinary tract symptoms and pelvic pain in men. It is commonly diagnosed in men over 50 and is the leading cause of urinary issues in men under 50.
Causes:
Bacterial Infections: Urinary tract infections or sexually transmitted infections like chlamydia and gonorrhea can lead to prostatitis.
Pelvic Muscle Disorders: Tightness or dysfunction in pelvic floor muscles may contribute to chronic pelvic pain syndrome.
Nerve Damage: Injury to nerves in the lower urinary tract due to surgery or trauma can cause inflammation.
Urinary Tract Abnormalities: Conditions like urethral stricture or bladder stones can increase risk.
Symptoms:
Pain or Burning Sensation During Urination: Discomfort while urinating is common.
Frequent Urination: An increased urge to urinate, especially at night.
Pelvic or Lower Back Pain: Persistent discomfort in the pelvic region or lower back.
Painful Ejaculation: Discomfort during or after ejaculation.
Flu-like Symptoms: Fever, chills, and body aches may occur in acute cases.
Prevention:
Safe Sexual Practices: Using protection and regular STI screenings help prevent bacterial causes.
Good Hygiene: Maintaining cleanliness can prevent the spread of infections.
Regular Check-ups: Routine medical examinations can help detect and manage conditions that may lead to prostatitis.
Early recognition and management of prostatitis are crucial to prevent complications. If symptoms arise, consulting a healthcare professional is essential for appropriate evaluation and care.
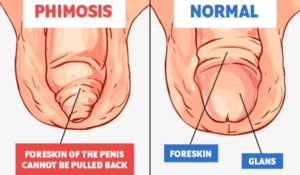
Phimosis is a condition where the foreskin of the penis cannot be retracted over the glans (head). This condition is common in infants and young children, often resolving naturally with age. However, in some cases, it persists into adolescence or adulthood, potentially leading to complications.
Causes:
Physiological Phimosis: Present at birth, the foreskin is naturally tight and adherent to the glans. It typically becomes retractable over time without intervention.
Pathological Phimosis: Results from scarring, infection, or inflammation, often due to poor hygiene, repeated infections, or trauma.
Symptoms:
Inability to Retract Foreskin: The primary sign of phimosis is the difficulty or inability to pull back the foreskin over the glans.
Swelling or Ballooning During Urination: Urine may cause the foreskin to balloon out due to the narrow opening.
Pain or Discomfort: Especially during erections, sexual activity, or urination.
Redness and Inflammation: The foreskin or glans may appear red, swollen, or tender.
Recurrent Infections: Such as balanitis (inflammation of the glans) or urinary tract infections.
Prevention:
Proper Hygiene: Gently cleaning under the foreskin with warm water can prevent infections and inflammation.
Avoiding Forceful Retraction: Especially in children, as this can cause tears and scarring.
Regular Medical Check-ups: Early detection and management of any foreskin issues can prevent complications.
Understanding phimosis is crucial for maintaining penile health. If symptoms arise or persist, consulting a healthcare professional is recommended for appropriate evaluation and guidance.
Scrotal eczema, also known as genital eczema, is a form of dermatitis affecting the skin of the scrotum. It manifests as redness, itching, and inflammation, often leading to significant discomfort.
Causes:
Skin Irritants: Exposure to harsh soaps, detergents, or personal care products can trigger eczema.
Allergens: Materials like latex in condoms or certain fabrics may cause allergic reactions.
Sweat and Heat: Excessive moisture and warmth in the groin area can exacerbate symptoms.
Stress: Emotional stress is known to provoke or worsen eczema flare-ups.
Underlying Skin Conditions: Conditions like atopic dermatitis or seborrheic dermatitis can affect the scrotal area.
Symptoms:
Itching and Burning: Persistent itchiness and a burning sensation are common.
Redness and Inflammation: The skin may appear red, swollen, and tender.
Dryness or Oozing: Affected areas might be dry and flaky or exhibit oozing in more severe cases.
Thickened Skin: Chronic scratching can lead to lichenification, where the skin becomes thick and leathery.
Prevention:
Gentle Hygiene: Use mild, fragrance-free cleansers and avoid harsh soaps.
Breathable Clothing: Wear loose-fitting, cotton underwear to reduce moisture buildup.Avoid Known Irritants: Identify and steer clear of products or materials that trigger symptoms.
Stress Management: Incorporate relaxation techniques to mitigate stress-induced flare-ups.
Recognizing and addressing scrotal eczema promptly can alleviate discomfort and prevent complications. Consulting a healthcare professional is advisable for accurate diagnosis and management.
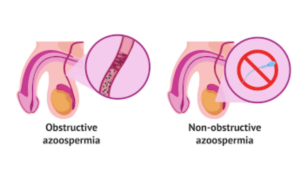
Azoospermia is a medical condition characterized by the complete absence of sperm in the ejaculate, making it a significant cause of male infertility. It affects approximately 1% of the male population and up to 10–15% of infertile men.
Causes:
Pretesticular Factors: Hormonal imbalances, such as low testosterone levels or pituitary gland disorders, can impair sperm production.
Testicular Factors: Genetic conditions like Klinefelter syndrome, Y-chromosome microdeletions, or damage from chemotherapy, radiation, or infections can lead to impaired sperm production.
Post-testicular Factors: Obstructions in the reproductive tract, such as blockages in the vas deferens or ejaculatory ducts, can prevent sperm from being present in the semen.
Symptoms:
Infertility: The primary symptom is the inability to conceive a child after a year of unprotected intercourse.
Low Semen Volume: Some men may notice a decrease in the volume of ejaculate.
Pain or Swelling: In certain cases, underlying conditions causing azoospermia may lead to discomfort or swelling in the testicular area.
Hormonal Imbalances: Symptoms such as decreased facial or body hair, reduced muscle mass, or decreased libido may be present due to hormonal issues.
Prevention:
Avoid Exposure to Toxins: Limiting exposure to harmful chemicals, radiation, and excessive heat can help maintain healthy sperm production.
Healthy Lifestyle: Maintaining a balanced diet, regular exercise, and avoiding illicit drugs and excessive alcohol can support reproductive health.
Regular Medical Check-ups: Early detection and management of conditions that could lead to azoospermia are crucial.
Understanding azoospermia is essential for men facing fertility challenges. If concerns arise, consulting a healthcare professional for appropriate evaluation and guidance is recommended.
Lymphogranuloma venereum (LGV) is a sexually transmitted infection caused by specific strains of Chlamydia trachomatis. It primarily affects the lymphatic system, leading to inflammation and swelling of lymph nodes, particularly in the groin area. LGV progresses through three stages, each with distinct clinical manifestations.
Causes:
Bacterial Infection: LGV is caused by invasive serovars L1, L2, or L3 of Chlamydia trachomatis.Transmission: The infection spreads through unprotected anal, vaginal, or oral sexual contact with an infected individual.
High-Risk Groups: Men who have sex with men (MSM) and individuals with HIV are at higher risk.
Symptoms:
Primary Stage: A small, painless ulcer or lesion appears at the site of infection, often unnoticed.
Secondary Stage: Swollen, tender lymph nodes (buboes) in the groin; fever; malaise; and, in some cases, rectal inflammation leading to discharge or bleeding.
Tertiary Stage: If untreated, chronic inflammation can lead to scarring, strictures, and permanent damage to genital or rectal tissues.
Prevention:
Safe Sexual Practices: Consistent use of condoms and dental dams during sexual activity reduces the risk of transmission.
Regular Screening: Routine STI testing, especially for high-risk groups, aids in early detection and treatment.
Partner Notification: Informing sexual partners ensures they can seek testing and treatment, preventing further spread.
Early recognition and management of LGV are crucial to prevent complications. If symptoms arise, consulting a healthcare professional is essential for appropriate evaluation and care.
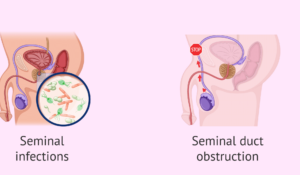
Oligospermia, also known as oligozoospermia, is a condition characterized by a low sperm count in the semen, which can impact male fertility. According to the World Health Organization, a sperm count below 15 million per milliliter is considered low.
Causes:
Hormonal Imbalances: Disruptions in hormones like testosterone can affect sperm production.
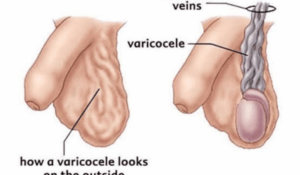
Varicocele: Enlarged veins in the scrotum can impair sperm quality.
Infections: Certain infections can interfere with sperm production or health.
Lifestyle Factors: Smoking, excessive alcohol consumption, drug use, and exposure to environmental toxins can reduce sperm count.
Medical Conditions: Obesity, stress, and certain medications can contribute to oligospermia.
Symptoms:
Difficulty conceiving a child.
Low sexual desire or other sexual dysfunctions.
Pain, swelling, or a lump in the testicular area.
Decreased facial or body hair, indicating hormonal issues.
Prevention:
Healthy Lifestyle: Maintain a balanced diet, exercise regularly, and avoid tobacco and excessive alcohol.
Avoid Heat Exposure: Limit exposure to high temperatures, such as hot tubs and saunas, which can affect sperm production.
Manage Stress: Chronic stress can interfere with hormone levels and sperm production.
Regular Check-ups: Routine medical examinations can help detect and address issues early.
Understanding oligospermia is crucial for addressing fertility concerns. If you suspect any symptoms or have difficulties with conception, consulting a healthcare professional is recommended for appropriate evaluation and guidance.
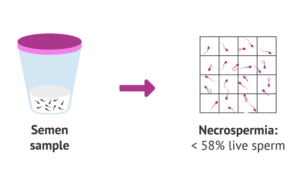
Necrospermia, also known as necrozoospermia, is a rare male fertility disorder characterized by a high percentage of dead or non-viable sperm in the semen. This condition significantly reduces the chances of natural conception, as the sperm are unable to fertilize an egg.
Causes:
Infections: Genital infections, such as sexually transmitted infections (STIs) or bacterial infections in the reproductive tract, can lead to sperm cell death.
Hormonal Imbalances: Disruptions in hormone levels, including testosterone, can impair sperm vitality.
Varicocele: Enlarged veins in the scrotum can increase testicular temperature, affecting sperm health.
Oxidative Stress: An imbalance between free radicals and antioxidants in the body can damage sperm cells.
Environmental Factors: Exposure to toxins, chemicals, or radiation can harm sperm viability.
Symptoms:
Infertility: Difficulty achieving pregnancy despite regular unprotected intercourse.
Abnormal Semen Characteristics: Such as increased viscosity or unusual coloration.Cap-Score
Low Sperm Count: A reduced number of sperm in the semen sample.
Reduced Sperm Motility: Sperm may be immotile or have poor movement, hindering their ability to reach and fertilize an egg.
Prevention:
Healthy Lifestyle: Maintain a balanced diet, exercise regularly, and avoid tobacco and excessive alcohol.
Avoid Heat Exposure: Limit exposure to high temperatures, such as hot tubs and saunas, which can affect sperm production.
Manage Stress: Chronic stress can interfere with hormone levels and sperm production.
Regular Check-ups: Routine medical examinations can help detect and address issues early.
Understanding necrospermia is crucial for addressing fertility concerns. If you suspect any symptoms or have difficulties with conception, consulting a healthcare professional is recommended for appropriate evaluation and guidance.
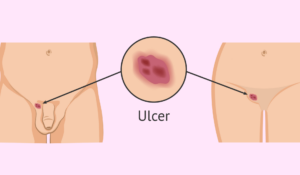
Chancroid, also known as soft chancre, is a sexually transmitted infection (STI) caused by the bacterium Haemophilus ducreyi. It is characterized by the development of painful genital ulcers and swollen lymph nodes in the groin area.
Causes:
Bacterial Infection: Chancroid is caused by Haemophilus ducreyi, a gram-negative bacterium that infects the genital area through microabrasions during sexual contact.
Transmission: The infection spreads through sexual activities, including vaginal, anal, and oral sex, with an infected individual.
Symptoms:
Painful Ulcers: Within 3 to 7 days after exposure, small, painful blisters form on the genitals or around the anus, which rapidly rupture to form shallow, open sores with ragged edges.
Swollen Lymph Nodes: About half of those infected develop enlarged, painful lymph nodes in the groin, which may become abscessed and rupture.
Discomfort During Urination and Intercourse: In women, ulcers may cause pain during urination and sexual intercourse.
Prevention:
Safe Sexual Practices: Consistent use of condoms and dental dams during sexual activity reduces the risk of transmission.
Limiting Sexual Partners: Reducing the number of sexual partners can lower the risk of exposure to STIs.
Regular STI Screenings: Routine testing for STIs, especially for sexually active individuals with multiple partners, aids in early detection and treatment.
Understanding chancroid is essential for maintaining sexual health. If you experience symptoms or suspect exposure, consult a healthcare professional for appropriate evaluation and guidance.
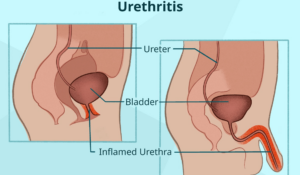
Non-Specific Urethritis (NSU), also known as Non-Gonococcal Urethritis (NGU), is an inflammation of the urethra not caused by gonorrhea. It is commonly associated with sexually transmitted infections (STIs) and can affect individuals of any gender, though symptoms are often more noticeable in men.
Causes:
Infections from bacteria like Chlamydia trachomatis, Mycoplasma genitalium, and Ureaplasma urealyticum.
Irritation from soaps, deodorants, or spermicides.
Physical trauma to the urethra from activities like vigorous sex or catheter use.
Symptoms:
Clear or white penile discharge.
Burning sensation during urination.
Itching or irritation inside the penis.
Pain and swelling in the testicles.
Prevention:
Practice safe sex by using condoms.
Limit the number of sexual partners.
Avoid irritants like harsh soaps or chemicals near the genital area.
Ensure proper hygiene and regular STI screenings.
Early detection and treatment of NSU are crucial to prevent complications. If you experience any symptoms or suspect exposure, consult a healthcare professional for appropriate evaluation and guidance.
About Sexual Problems
Sexual dysfunction refers to persistent issues that impede an individual’s ability to experience satisfaction during sexual activity. These problems can affect any phase of the sexual response cycle, including desire, arousal, orgasm, and resolution. Both men and women can experience sexual dysfunction, which may stem from physical, psychological, or relational factors.
Causes of Sexual Problems
Causes of Sexual Problems:
Physical Factors:
Cardiovascular diseases affecting blood flow.
Diabetes leading to nerve damage.
Hormonal imbalances, such as low testosterone or estrogen.
Neurological disorders like multiple sclerosis.
Chronic illnesses, including kidney or liver failure.
Side effects from medications, including antidepressants and antihypertensives.
Substance abuse, including alcohol and recreational drugs.
Psychological and Emotional Factors:
Stress and anxiety related to work or personal life.
Depression affecting libido and energy levels.
Past sexual trauma or abuse.
Relationship issues, including lack of trust or communication.
Body image concerns leading to self-consciousness.
Lifestyle and Other Factors:
Sedentary lifestyle contributing to poor circulation.
Poor diet lacking essential nutrients.
Smoking leading to vascular problems.
Excessive alcohol consumption impairing sexual response.
Symptoms of Sexual Issues
Symptoms of Sexual Problems:
In Men:
Difficulty achieving or maintaining an erection.
Premature or delayed ejaculation.
Reduced sexual desire.
Pain during ejaculation.
In Women:
Lack of sexual desire or arousal.
Inability to achieve orgasm.
Pain during intercourse (dyspareunia).
Vaginal dryness leading to discomfort.
Common to Both Genders:
Avoidance of sexual activity.
Emotional distress related to sexual performance.
Strained relationships due to sexual dissatisfaction.
Addressing sexual dysfunction often requires a comprehensive approach, considering both physical health and emotional well-being. Open communication with healthcare providers and partners is essential for effective management.
Treatments
Contact Us
- Shah Market Opp. PNB bank, Shahbad Gate, Rampur U.P 244901
- +91 99274 25447
- iinfo@drmyu.com
